Oral Health
Oral Health
Since 1974 | Patient Referral Program | Locally Owned
Since 1974Patient Referral ProgramLocally Owned
Oral Health
What does the phrase "oral health" mean to you? No new cavities at your dental checkup? That's certainly part of it. But it's really so much more than a lack of tooth decay. Good oral health means a mouth that's free of disease - which can range all the way from mild gingivitis (gum inflammation) to oral cancer; a bite that functions well enough for you to eat without pain and get ample nutrition; and a smile that lets you express your happiest emotions with confidence. Simply put, oral health is a crucial component of your overall health and well-being.

What You Can Do to Stay Healthy
One of the most important things you can do to safeguard your oral health is to maintain a daily oral hygiene routine that effectively removes plaque from your teeth. It's the bacteria that thrive in the plaque biofilm that cause so many oral health problems. Effective oral hygiene involves brushing your teeth twice daily with a fluoride toothpaste and flossing at least once per day to remove plaque from between the teeth.
Nutrition and lifestyle choices also play an important role. You don't have any control over hereditary factors that may predispose you to gum disease - but you do have control over how much sugar you eat and when you eat it; how often you exercise; whether you smoke; and how often you visit the dentist.
How Dentistry Can Help
If you only see a dentist when problems arise, you may be missing out on some important benefits! As doctors who specialize in oral health, dentists offer a wide range of preventive services. At your regular exams, for example, you will be checked for any signs of oral cancer, tooth decay, gum disease, and other oral infections; hard-to-reach deposits from your teeth will be cleaned; and you can get answers to any questions you have on topics ranging from oral hygiene issues to the connection between oral health and systemic diseases.
So please don't wait for a serious problem to come up before you make an appointment at the dental office. Having regular checkups could save you lots of time, aggravation, and cost in the long run. It could even save your teeth! Working together, we can take proactive steps toward a healthy future.
Brush and Floss. You should brush at least twice a day and floss at least once daily. This will help remove plaque, a bacteria-laden bio film, from the surfaces of your teeth. The bacteria in plaque can turn sugars from food into acids, which attack the tooth's enamel and cause tooth decay. Some bacteria can also cause gingivitis and other gum diseases.
Make sure you're getting the proper amount of fluoride. Fluoride strengthens tooth enamel — it's essential for children's developing teeth, and helps prevent decay in both kids and adults. Even if your municipal water is fluoridated, you should always use fluoride toothpaste. If more fluoride is needed, it can be applied directly to your teeth at the dental office.
Limit between-meal snacks. Sugary snacks are the perfect fuel for decay-causing bacteria — and when eaten throughout the day, they keep the acid constantly on the attack. So give your mouth a break, and (if you allow them) limit sugary treats to mealtime.
Use an appropriate mouth rinse — especially if you're at increased risk. Therapeutic mouth rinses do more than temporarily mask bad smells or tastes in your mouth — they can improve your overall oral hygiene. While some over-the counter products offer primarily “cosmetic” benefits, therapeutic rinses contain anti-bacterial and anti-carcinogenic (cavity-fighting) ingredients. Using a therapeutic mouth rinse has been proven to control plaque bacteria and prevent cavities better than brushing and flossing alone.
Quit tobacco. Whether smoked or smokeless, tobacco use greatly increases your risk of oral cancer, gum disease, and tooth.
decay (not to mention heart disease and lung cancer… but you already knew that). If you use tobacco, ask us how to quit now.
Examine your mouth regularly. Once you've established a regular routine, you'll quickly recognize any changes in your mouth — like chipped teeth, red or swollen gums, or unusual sores. If you find something of concern, let us know. Early treatment offers the best chance to remedy many problems.
A major goal of modern dentistry is to help you keep your teeth and gums healthy for a lifetime. By following a conscientious program of oral hygiene, you have the best chance at making this goal a reality.
Related Articles
Aging & Dental Health
Top
Today, Americans are not only living longer — we're also retaining our natural teeth longer than ever before. But this rosy picture isn't free of thorns: Older adults tend to require increasingly complex dental treatments; are often more prone to contracting certain diseases; and sometimes find it challenging to keep up with daily oral health practices.
Yet maintaining good oral hygiene is critically important as we age. When problems occur in the mouth, they can cause difficulty chewing, swallowing, speaking and smiling — basic functions which can affect both physical and social well-being. It's possible that medications prescribed for other diseases can adversely affect a person's oral health; it's also possible that a decline in oral health can worsen existing maladies (such as diabetes), or even cause systemic (whole-body) inflammation. What other special dental issues do older people face — and what can be done about them?

Dental Concerns for Older Adults
If you think cavities are just for kids — think again! A recent study found that nearly one-third of people over 65 had untreated dental caries (cavities). In older people, these are found not only in the crown (chewing surface) of the tooth, but also in the root, which may become exposed due to gum recession. Regular dental checkups are the best way to find and treat dental caries; left untreated, they can cause pain, require more complex procedures, and eventually lead to lost teeth.
Gum disease is another major oral health issue faced by older people — and it's presently the leading cause of tooth loss in adults. The disease is caused by plaque bacteria, which thrive on the sticky biofilm that clings to the surface of teeth when they aren't properly cleaned. Poor-fitting dentures can make the problem worse, as can the presence of certain diseases (such as diabetes or cancer).
Sometimes, decreased mobility (due to arthritis or similar conditions) makes routine brushing and flossing more difficult. Special brushes with larger grips and floss holders can help make daily cleaning easier; additionally, therapeutic mouthrinses may be prescribed. In-office treatments can also be effective in bringing gum disease under control.
Oral cancer is a concern at any age, but it's 7 times more likely to show up in a person over 65 — and it causes more deaths in older Americans than skin cancer does. Early detection offers the best chance at controlling the disease, and improves survival rates significantly. A thorough screening for oral cancer should be a part of every older person's routine dental checkup.
Dry mouth (xerostomia) isn't just an annoyance — it can be harmful to your oral health. Aside from its lubricating qualities, saliva contains beneficial digestive enzymes, acid neutralizers, and bacteria-fighting agents. A number of factors may cause the body to produce less saliva than normal — but in older adults, this problem is often due to side effects from prescription or over-the-counter medications. If you're experiencing chronic dryness of the mouth, it's sometimes possible to change your medication, and/or use products designed to relieve these symptoms.
Oral Hygiene For Life
It was once commonly believed that dental problems and the loss of teeth were an inevitable consequence of aging. But here's the fact: Age itself isn't a risk factor for tooth loss; properly cared for, your teeth can last a lifetime. However, it's true that the mouth does change as you age. How can you give yourself the best chance of keeping your natural teeth? You guessed it: Maintain a regular practice of good oral hygiene!
Brush twice a day with a soft-bristled toothbrush — use one with a special grip, or an electric brush, if it helps. Clean in between your teeth with floss, or another type of interdental cleaner, at least once a day. If you wear dentures, regularly clean and care for them as instructed. Eat healthy foods and drink plenty of water. And don't forget to have regular dental exams so that little problems don't turn into major headaches!
Related Articles
Antibiotic Premedication for Dental Treatments
Antibiotics are widely prescribed to control bacterial infections. Sometimes they are given before a medical or dental procedure, to prevent a possible infection from occurring; this practice is called "antibiotic prophylaxis." In the recent past, physicians and dentists advised that people with certain medical conditions - including a number of heart problems and several types of bone or joint replacements - should always take antibiotics before many routine dental procedures. Today, their advice may be different.
A growing body of evidence now indicates that far fewer patients need to take this preventive step than was previously thought. As a result, the guidelines for prescribing antibiotic prophylaxis have recently changed - and they may do so again in the future. Why are the recommendations changing - and what do you need to know about taking antibiotics before coming to the dental office?
The Risk of Infections
We all know that bacteria - both helpful and harmful types - thrive in many parts of the body, including the mouth. Whenever circumstances make it possible for these microorganisms to enter the bloodstream, there's a slight risk that a bacterial infection may develop. This could occur in many dental procedures - and it could also occur during routine activities like chewing, brushing and flossing. In most cases, the risk is so small that the chance of a having bad reaction to antibiotics (while rare) is far greater than the chance of developing an infection; therefore, antibiotics aren't routinely used.
Some people, however, need to take extra precautions before having dental procedures. If you have been treated for some types of heart disease, or have had certain orthopedic procedures (including total joint replacement), we may advise taking antibiotics to protect against even a remote chance of infection. Recommendations are made on an individual basis, taking into account your medical history and a clinician's healthcare experience.
Guidelines for Antibiotic Premedication
Prophylactic antibiotics might be recommended before dental procedures if you have one or more of the following heart conditions:
- A heart transplant
- Artificial heart valves
- A history of infective endocarditis
Some types of congenital heart problems - particularly if they haven't been completely repaired, or if their treatment involves prosthetic material if you have undergone a joint replacement procedure, prophylactic antibiotics might be recommended if you also have one or more of the following risk factors:
- A systemic inflammatory disease such as rheumatoid arthritis or lupus erythematosis
- A weakened immune system resulting from HIV, cancer, radiation or chemotherapy, or another cause
- Insulin-dependent (type I) diabetes or hemophilia
- A history of previous infection in a prosthetic joint
- Undernourishment or malnourishment
There are other circumstances where taking prophylactic antibiotics would be a prudent step; there are also a number of situations where these medications might have been recommended in the past, but aren't currently required in all cases. For example, the presence of a benign heart murmur, a pacemaker or defibrillator, and certain heart diseases or congenital defects don't automatically mean that antibiotic prophylaxis will be needed.
In recent years, reports of drug-resistant bacteria and harmful side effects from some medications have increased public awareness of the consequences of overusing antibiotics. Fortunately, new scientific research is helping healthcare professionals make better, evidence-based treatment decisions on antibiotic use. If you have questions about whether you should take antibiotics before dental procedure, don't hesitate to ask.

Related Articles:
Bad Breath
Bad Breath, or halitosis, is an embarrassing problem that affects millions. To combat it, many people use breath mints, chewing gum, sprays and mouthwashes. In fact, Americans spend billions of dollars each year on these products — even though they offer only a temporary fix. Getting rid of persistent foul odors on the breath in a lasting way requires a little detective work on the part of dental professionals.
Bad breath can affect anyone temporarily — think of “morning breath,” or the way your mouth smells after eating onions or drinking coffee. Some people, however, exhale noticeably unpleasant odors throughout the day, every day. That's when it is important to find the cause of the problem, so a lasting solution can be achieved.
Causes
Most often, bad breath originates in the mouth, from trapped food particles that are then processed by oral bacteria. The most common location for mouth-related bad breath is the back of the tongue, where large quantities of naturally occurring bacteria can thrive on food remnants, dead skin cells and post-nasal drip (mucus coming down your throat from the nose). The waste products of these bacteria include volatile sulfur compounds (VSCs), which have a smell resembling rotten eggs. Other places where bacteria and food particles can be trapped are between the teeth, beneath the gums, and in oral appliances or dentures. Poor oral hygiene sets the stage for these problems, as well as for tooth decay and gum disease, which can also cause foul odors.
It's possible for other health conditions and habits to affect your breath. Halitosis may occur in people who have a sinus or bronchial infection, an oral yeast infection (which can be caused by antibiotic use), or even a systemic (general body) disease such as diabetes, kidney failure or a liver malfunction. A chronically dry mouth (xerostomia), which is often a side effect of certain medications, and tobacco use can also contribute to this problem. Even stress, dieting and hormonal changes can affect your breath.
How Dentistry Can Help
Since bad breath most often originates in the mouth, the dental office is the best place to start in your quest for consistently better-smelling breath. After a thorough examination, any of the following might be recommended:
Oral hygiene instruction. It might be that you could benefit from a demonstration of how to brush and floss more effectively, or how to better clean your dentures. You can also be instructed on how to use a tongue scraper to clean the back of your tongue if necessary.
- Professional dental cleaning. Food particles, bacteria and calcified deposits can become trapped where you can't reach them — but special dental instruments can. Regular professional cleanings are a great way to promote good oral health in general and good-smelling breath in particular.
- Treatment of tooth decay. Bad breath may be caused by large, open cavities that need to be filled, or old, defective fillings that need to be repaired.
- Treatment of gum disease. More advanced forms of gum disease cause the gums to separate from the teeth, forming pockets in which bacteria can thrive. If you have gum disease, you may need periodontal (gum) therapy, which can include a deep cleaning of the roots of your teeth, antibiotics, and, in advanced cases, periodontal surgery.
- Treatment of infection. Infection that doesn't originate in your mouth needs to be treated by the appropriate medical professional. Whatever the cause of your bad breath, we are here to make sure you get the treatment you need.
Related Articles
Blood Pressure Medications & Your Gums
Top
Before prescribing any medications — even lifesaving ones, such as those used to reduce blood pressure or prevent epileptic seizures — your health care professionals carefully weigh the benefits a drug offers against the possible risks of taking it, including its potential side effects. In most cases, the side effects are relatively slight: for example, drowsiness, an upset stomach, or minor aches. But in some individuals, particular drugs may produce side effects that are more troublesome.
This is sometimes the case with a class of drugs called calcium channel blockers (CCBs), which are commonly used to treat high blood pressure (hypertension) and certain other heart conditions. Some people who take these medications experience a condition called gingival hyperplasia, or an overgrowth of gum tissue. This effect has also been seen in some epileptics who take an anti-seizure medication called phenytoin.
Possible Side Effects
CCBs work by dilating (widening) the blood vessels, which makes it easier for the heart to pump blood. But in a small percentage of people, they also cause changes in the gums. Gum tissue may become thick and lumpy, and it may sometimes extend abnormally and start to cover the teeth. This change in appearance can cause social embarrassment, as well as discomfort and difficulty in chewing.
The overgrowth of gum tissue also makes it difficult or impossible to clean the spaces between teeth. This can cause a rapid deterioration in oral hygiene that may lead to full-blown gum disease if not treated promptly. And since poor oral hygiene is itself a contributing factor in gum overgrowth, the condition can easily spiral out of control.
In addition, some CCBs also reduce saliva flow. This may not only cause the mouth to feel dry, but may also severely reduce saliva's protective effects on the teeth and gums.

What to Do About Gum Overgrowth
It's always a good idea to tell your health care providers about any side effects you may be experiencing as soon as you notice them. However, even though gum tissue overgrowth may be a worrisome issue, it doesn't mean you should stop taking your blood pressure medication! There are several options for controlling this condition, which should be discussed with all members of your medical team.
With your doctor's consent, it may be possible for you to change your dosage or switch to a different blood pressure medication that produces fewer side effects. It can take a few months for your gums to return to normal after the change, while you are maintaining good oral hygiene at home. But even if it's not possible for you to change your medication, there are a number of in-office treatments that can be used to help alleviate the problem.
Non-surgical treatments like scaling and root planing (a type of deep cleaning) are sometimes the first step to controlling gum overgrowth. These relatively minor procedures can dramatically improve your overall oral hygiene. If necessary, they may be followed by surgical treatments to remove overgrown tissue and eliminate periodontitis — a serious condition which, if left untreated, could result in tooth loss.
In addition to regular dental cleanings, you will need to be extra vigilant at home: proper brushing technique and the use of interdental cleaners (such as floss) are needed to clean the spaces between teeth is a must. Your progress will be monitored at follow-up dental visits as needed.
While gum tissue overgrowth may seem a daunting problem, experience has shown that it can be successfully controlled by initial periodontal therapy, good at-home care, and frequent follow-up visits. Meanwhile, you should continue to follow all of your doctors' recommendations for maintaining a healthy blood pressure.
Related Articles
Diabetes & Oral Health
Diabetes is a group of chronic inflammatory diseases that affect the body's ability to process sugar. If you have diabetes, it is particularly important to maintain excellent oral health. That's because diabetics are more prone to oral infections such as periodontal (gum) disease, which can result in tooth loss if left untreated. Conversely, the presence of gum disease can make it harder for people with diabetes to control their blood sugar levels.
Periodontal disease is a chronic ailment that is also associated with an elevated level of systemic (whole-body) inflammation. Like diabetes, it may have wide-ranging consequences outside the mouth — possibly increasing a person's chance of experiencing major cardiovascular events (such as heart attack or stroke) or adverse pregnancy outcomes (low birth weight and pre-term delivery). So perhaps it's not surprising that a growing body of evidence suggests the two diseases are related.
Two Diseases With A Lot In Common
It has long been recognized that having diabetes is a risk factor likely to increase the severity of periodontal disease. That's because diabetes reduces the body's resistance to infection, making diabetics more susceptible to both bacterial and fungal infections. Likewise, evidence shows that having serious gum disease (periodontitis) is likely to result in worsening blood glucose control in diabetics; it can also increase the risk of diabetic complications. So, what's the connection?
While no one is sure at present, the two diseases seem to share some common pathways and disease-causing mechanisms. Both are associated with the process of inflammation and the immune response. Inflammation itself — often signaled by pain, heat and redness — is evidence of the body's immune system at work, attempting to fight disease, repair its effects, and prevent it from spreading. Chronic or prolonged inflammation, however, can lead to serious problems in different parts of the body and a decline in overall health.
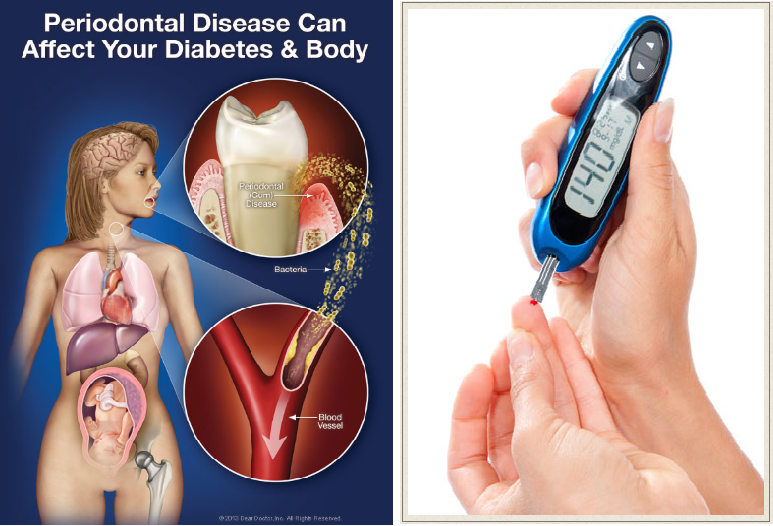
What does this mean to you? According to one large study, if you're diabetic, your risk of dying from heart attack is over twice as great if you also have severe periodontitis — and for kidney disease, your risk is 8.5 times higher! Plus, uncontrolled periodontal disease makes it six times more likely that your ability to control blood sugar levels will get worse over time. So not only can having one condition put you at risk for worsening the other — having both can cause a significant deterioration in your overall health.
A Two-Way Street
While diabetes can't be cured, it's possible to manage the disease on a long-term basis. And here's some good news: Clinical studies show that diabetics who get effective treatment for their periodontal disease also receive some significant benefits in their general health. Many exhibit better blood glucose control and improved metabolic functioning after periodontal treatment.
What kinds of treatments might be needed? While much depends on the individual situation, some typical procedures might include: scaling and root planing (a deep cleaning that removes plaque bacteria from teeth, both above and below the gum line); antibiotic therapy; and oral hygiene self-care instruction.
Likewise, if you're at risk for diabetes but haven't yet developed the disease, there are some things you can do to forestall it. While there is a significant genetic component, a major risk factor for diabetes is being overweight — so keeping your weight under control will better your chances of avoiding it. High levels of triglycerides or low levels of HDL (good) cholesterol are also risk factors. These may respond to changes in your diet — like cutting out sugary drinks and eating healthier foods. Also, high blood pressure coupled with an inactive lifestyle puts you at greater risk. Here, moderate exercise can help.
When you come to our office, be sure to let us know if you're being treated for, or are at risk of developing diabetes. And if you are managing the disease, remember that it's more important than ever to maintain good oral health.
Related Articles
Dry Mouth
Top
Everybody gets a dry mouth from time to time. Temporary mouth dryness can be brought on by dehydration, stress, or simply the normal reduction in saliva flow at night. But persistent mouth dryness, a condition known as xerostomia, is cause for concern.
Xerostomia occurs when your salivary glands, which normally keep your mouth moist by secreting saliva, are not working properly. A chronic lack of saliva has significant health implications. For one thing, it can be difficult to eat with a dry mouth; tasting, chewing and swallowing may also be affected. This could compromise your nutrition. Also, a dry mouth creates ideal conditions for tooth decay. That's because saliva plays a very important role in keeping decay-causing oral bacteria in check and neutralizing the acids these bacteria produce; it is the acid in your mouth that erodes tooth enamel and starts the decay process. A dry mouth can also cause bad breath.

Possible Causes
There are several possible causes for xerostomia, including:
- Medications. For most people suffering from dry mouth, medications are to blame. According to the U.S. Surgeon General, there are more than 500 medications (both prescription and over-the-counter) that have this side effect. Antihistamines (for allergies), diuretics (which drain excess fluid), and antidepressants, are high on the list of medications that cause xerostomia. Chemotherapy drugs can also have this effect.
- Radiation Therapy. Radiation of the head and neck can damage salivary glands—sometimes permanently. Radiation to treat cancer in other parts of the body will not cause xerostomia.
- Disease. Some systemic (general body) diseases can cause dry mouth. Sjögren's syndrome, for example, is an autoimmune disease that causes the body to attack its own moisture-producing glands in the eyes and mouth. Other diseases known to cause dry mouth include diabetes, Parkinson's disease, cystic fibrosis and AIDS.
- Nerve Damage. Trauma to the head or neck can damage the nerves involved in the production of saliva.
Getting Relief
If you are taking any medication regularly, it's possible that your physician can either suggest a substitute or adjust the dosage to relieve your symptoms of dry mouth. If this is not possible or has already been tried, here are some other things you can do:
Sip fluids frequently.
This is particularly helpful during meals. Make sure what you drink does not contain sugar and isn't acidic, as these will both increase your risk of tooth decay. All sodas, including diet varieties, should be avoided, as they are acidic and attack the tooth surface.
- Chew sugarless gum. This will help stimulate saliva flow if your salivary glands are not damaged. Choose a variety that contains xylitol, a natural sugar substitute that can be protective against tooth decay.
- Avoid drying/irritating foods and beverages. These include toast and crackers, salty and spicy foods, alcohol and caffeinated drinks.
- Don't smoke. This can dry out the mouth and also increase your risk of gum disease.
- Use a humidifier. Running a cool-mist humidifier at night can be soothing.
- Use saliva stimulants/substitutes. There are prescription and over-the-counter products that can either stimulate saliva or act as a substitute oral fluid. We can give you some recommendations.
- Practice good oral hygiene. Brush at least twice a day with a fluoride toothpaste; this will remove bacterial plaque and add minerals to strengthen your teeth. Don't forget to floss.
- Have an exam/cleaning.
If you have dry mouth, it's more important than ever to maintain your regular schedule of visits to the dental office. Please be sure to let us know what medications you are taking, particularly if there have been any changes recently. We will do our best to help relieve any dry-mouth symptoms you are experiencing.
Related Article
Eating Disorders & Oral Health
Millions of people in the United States, particularly teenage girls and young women, suffer from health-threatening eating disorders, and dentists are often the first to spot the signs. Why? The repeated, self-induced vomiting that characterizes bulimia nervosa has a pronounced effect on teeth. Anorexia nervosa (self-starvation) can also have some noticeable effects on oral health.

More than 90% of those with bulimia experience tooth erosion. This is caused by acid from the stomach, which can dissolve the enamel when it comes in contact with teeth during vomiting. Teeth that have lost enamel can appear worn, chip easily, and become sensitive to hot and/or cold. Of course, acid erosion can also affect people who drink a lot of soda, sports drinks and energy drinks — even the diet varieties. But acid erosion in bulimics has a particular pattern: It is evident on the upper front teeth, particularly on the tongue side and biting edges. The bottom teeth, on the other hand, tend to be protected by the tongue when a person throws up.
Once enamel is lost, it can't grow back. But the damage can be repaired with various restorative techniques including veneers and/or crowns. The best treatment will be determined by how extensive the damage is, which in turn depends on how frequently the person has engaged in binge-purge behavior.
To protect teeth in the short term, it is important not to brush them immediately after vomiting as this can scrape off more of the softened enamel. It is better to rinse with water to which a little baking soda has been added, which neutralizes the acid. Even a plain water rinse is helpful. Sometimes a sodium fluoride mouthrinse is recommended to strengthen the enamel and reduce its loss.
Erosion is not the only sign of an eating disorder that a dentist or hygienist may notice. In severe cases the salivary glands can become enlarged, causing the sides of the face under the ears to look puffy. Also, the throat, back of the tongue and roof of the mouth can appear reddened or otherwise traumatized from the use of fingers or other objects to induce gagging. Soft tissues of the mouth can also be damaged by acid.
Only about 20% of anorexics experience tooth erosion, but there are other signs that may become apparent in the dental office. Nutrition and hygiene suffer in general, which in turn can mean more tooth decay and gum disease. There is also considerable overlap between anorexia and bulimia.
If you are struggling with an eating disorder or believe that a loved one is, please let your healthcare professionals know. We will make sure you get the help you need for healthy teeth and a healthy life. You can also visit the National Eating Disorders Association for some helpful information.
Related Articles
Fluoride
Fluoride is a mineral that is naturally present to some degree in both fresh and salt water sources. Its major dental benefit is that it is readily incorporated into the teeth's mineral structure, thereby making them stronger and more decay-resistant. Fluoride can even reverse tiny cavities that are starting to form. Less tooth decay means you have a better chance of avoiding significant dental treatments — and keeping your natural teeth for life.
The great majority of toothpastes sold today contain fluoride, because it's an effective, easy and inexpensive way to prevent tooth decay and promote oral health. Because of its proven health benefits, fluoride is often added to municipal water supplies to bring them to the current recommended level of 0.70 parts per million. In fact, the federal Centers for Disease Control and Prevention recently named community water fluoridation as one of the most significant public health achievements of the 20th century.
Making Fluoride Available to the Teeth
Fluoride can be delivered to teeth in two ways: topically (on the surface) and systemically (through the body). The first method helps people of all ages; the latter is only beneficial in childhood while the permanent teeth are forming beneath the gum line — up to about age 9.
Fluoride ingested in drinking water can reach teeth both ways. When swallowed, it travels through the body and becomes incorporated into developing teeth; it also stays in the mouth throughout the day in a very low concentration. Toothpaste and mouthwashes provide higher concentrations over shorter periods of time. Fluoride can also be applied directly to the teeth at the dental office; children who get their water from unfluoridated sources may be prescribed a fluoride supplement in the form of pills or drops.

How Much Do You Need?
The amount of fluoride you need varies according to your particular risk for decay, which is determined by many factors: your body's own biochemistry, your diet, the amount of fluoride you come into contact with daily, and the effort you put into your own oral hygiene. If you maintain an effective daily routine of brushing and flossing, and avoid sugary and/or acidic foods and beverages, your decay risk will likely be low. If you are lax about oral hygiene, drink soda and snack throughout the day, your risk will be much higher.
Poor oral hygiene and constant intake of sweets make an ideal environment for decay-causing bacteria, which need sugar to thrive. In the process of digesting that sugar, they create tooth-eroding acids as a byproduct. And if you drink beverages that are already acidic — soda, sports drinks, energy drinks, even some fruit juices — you are applying those tooth-destroying acids directly to your teeth without using bacteria as a middleman. In that case, you might benefit from fluoride treatments at the dental office and/or regular use of a fluoride mouth rinse.
However, there is such a thing as too much fluoride — particularly when it comes to children. If developing teeth absorb too much fluoride, they can become permanently stained or even pitted — a condition referred to as enamel fluorosis. It is not dangerous, but may require cosmetic dental work. That's why young children should not be allowed to swallow fluoride toothpaste. Adults who take in excessive fluoride throughout their lifetimes may become more prone to bone fractures or tenderness, a condition known as skeletal fluorosis. Severe forms of enamel or skeletal fluorosis are not common in the United States. Still, given that excessive doses of fluoride could cause problems, it's best to consult a dental professional on the most appropriate products for you and your child to use.
Related Articles:
Geographic Tongue
Geographic tongue is characterized by harmless lesions, or patches, that can suddenly materialize on the tongue's top surface. The condition gets its name from the physical appearance of the lesions, which resemble smooth, red islands, possibly rimmed with white. Their smoothness comes from the absence of the tiny bumps or “papillae” that normally cover the entire surface of the tongue. These variations in color and texture give the whole tongue a map-like appearance.
The pattern on the tongue can change daily as the lesions appear to move or migrate, healing in one spot only to reappear in another. That's why the medical term for this condition is benign migratory glossitis. It's scary looking, but does not compromise a person's health.
Discomfort from the condition can sometimes be relieved with over-the-counter pain relievers; mouthrinses containing anesthetics, antihistamines, or steroids; and by avoiding certain irritants such as tobacco, alcohol, and foods that are spicy, salty or acidic.
No one knows exactly what causes geographic tongue. Some factors that may play a role include vitamin B deficiency, irritation from alcohol or spicy foods, and genetics.
This condition can be diagnosed simply by examining your tongue; laboratory tests are usually not necessary. Geographic tongue normally resolves on its own, but a dental professional should be consulted if you notice any changes in your tongue's appearance.

Missing Teeth
If you are missing one or more of your adult teeth, you're not alone — an estimated 178 million Americans have the same condition. Many try to get along without all of their teeth, and suffer from some of the familiar problems that go with the territory: smiles that don't look as appealing as they once did, problems eating certain foods, and awkwardness or embarrassment in social situations.
Yet there are other problems associated with tooth loss that are less obvious, but could have more of an impact on your health. These include nutritional difficulties, oral health issues, and bone loss.
Nutritional Difficulties
It is well established that eating plenty of fruits and vegetables and avoiding highly processed foods are essential parts of good nutrition. But many foods become difficult to chew if you have missing teeth — and those “challenging” foods are often the same ones that offer the greatest nutritional value. Softer foods are easier to eat, but they are often highly processed, and offer little nutritional value. Along with the possibility of malnourishment, a poor diet can lead to a compromised immune system and a decline in overall health.
Oral Health Issues
If you have only one or two missing teeth, you may not feel an urgent need to replace them now. Yet the problems that stem from missing teeth don't get better — and in time, they can get much worse. Teeth aren't fixed solidly in the jaw; instead, wheneven one tooth is missing, the remaining teeth tend to “drift” into new positions. This can cause a cascade of oral health problems, including unstable tooth positions, excessive tooth wear, bite problems, a greater chance of developing tooth decay and periodontal disease — and the loss of even more teeth.
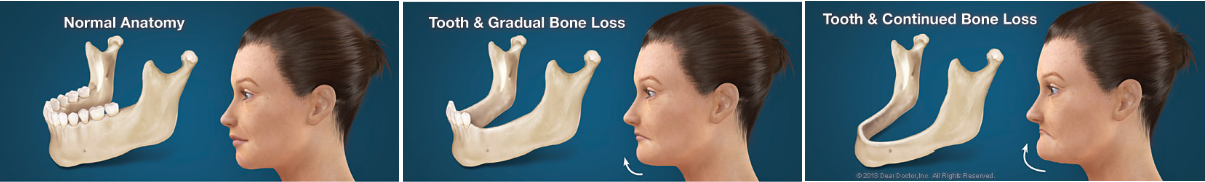
Bone Loss
You can't see the bone inside your jaw — but the consequences of bone loss are very real. Bone tissue needs stimulation to maintain its volume and density. When teeth are lost, the jaw bone that once supported them loses stimulation and begins to deteriorate. It can lose one-quarter of its width in just one year, and even more as time passes. As the jaw becomes smaller, facial height (the distance from nose to chin) decreases, and facial features lose support. The chin rotates forward, the corners of the mouth turn downward (as if frowning), and the cheeks can appear hollow. Loss of bone in the jaw can give you the appearance of being many years older than you actually are.
The consequences of tooth loss are very real, even if they are less visible than a gap in your smile. That's why it is so important not to put off the replacement of missing teeth.
Related Articles:
Nutrition & Oral Health
You probably already realize that maintaining a balanced diet offers a host of benefits to your overall health. But did you know diet also directly affects the health of your teeth and gums? It all starts before birth, as a baby's teeth begin forming in the sixth week of pregnancy and mineralizing in the third or fourth month. During this time, an expectant mother needs to take in lots of calcium (the major component of teeth) along with vitamin D, phosphorous and protein. Dairy products including milk, cheese, and yogurt have all of these. Broccoli and kale also have calcium, while meats are good sources of protein and phosphorous. These foods are also important for children, whose teeth continue to develop and mineralize through the teen years.
Throughout life, oral tissues are constantly recycling; they need a variety of nutrients to support this process. It's equally important to recognize that nutritional deficiencies — a particular concern among older adults who have lost teeth — can reduce resistance to disease and hinder your ability to fight infection. Studies have consistently found that a high intake of fruits and vegetables reduces the risk for oral cancer — as well as other types of cancer. That's why eating a nutritious diet is important for oral health — as well as general health — at any age.
Eating Healthy
What's the best diet for you? That depends mainly on your age, gender, height, weight and level of physical activity. But in general, a health-promoting diet is based on the concepts of:
* Variety.
No single food can meet all of the daily nutrient requirements. Eating lots of different foods also makes meals more interesting.
* Balance.
We need to eat the recommended amounts of foods from specific categories on a daily basis. Find out what your specific needs are at www.choosemyplate.gov
Choose MyPlate
ChooseMyPlate.gov
provides practical information to individuals, health professionals, nutrition educators, and ...
* Moderation.
Don't supersize it. Foods and beverages should be consumed in serving sizes that are appropriate to meet energy needs while controlling calories, fat, cholesterol, sodium, and — particularly important in the dental arena — sugar.
Protecting Your Teeth
Your diet (which includes what you drink) plays a major role in tooth decay and enamel erosion. Your mouth is naturally hospitable to all kinds of bacteria. Some of these microorganisms are helpful and some are harmful, and many of the harmful ones thrive on a steady supply of sugar. As they process sugar from your diet, these bacteria produce acids that can eat into the enamel of your teeth, forming small holes called cavities. If left untreated, tooth decay can worsen, become quite painful, and threaten the survival of teeth
That's why it is important to avoid food and drinks with added sugar. If you have a sugar craving (and we all do from time to time), choose fresh fruit or yogurt instead of a donut or candy bar. Fortunately, there is no evidence that sugars in whole grain foods, whole fruits and vegetables, and in starch-rich staple foods like bread, rice and potatoes are harmful to teeth.
Soft drinks, however, are a double whammy for teeth; many not only contain lots of sugar — up to 10 teaspoons per 12-ounce can — but they are also highly acidic. This means they erode teeth on contact, even before the bacteria in your mouth have processed the sugar these drinks contain. But even if they are sugar-free, the acid can still harm your teeth. So it might be best to avoid soda, sports drinks, energy drinks and canned iced tea. If you do occasionally have a soda, swish some water in your mouth afterwards — but don't brush your teeth for at least an hour! Doing so could make it easy for tooth enamel, already softened up by acid, to be eroded away by brushing.
Drinking lots of water can help you maintain a healthy supply of saliva, which protects teeth by neutralizing acid. You can also neutralize the acid in your mouth after a sugary snack by following it up with a piece of cheese.
Finally, remember that it's not just what you eat that affects the level of acidity in your mouth — it's also when. Snacking throughout the day, especially on chips, crackers, cookies or candy, means that your saliva never gets the chance to neutralize the harmful acids being produced. So if you eat sweets, do it only at mealtimes. As an added incentive, you may find this helps you maintain a healthy weight, too!

Related Articles:
Oral Cancer
Cancer is a scary word, but the more you know about it, the better able you will be to protect yourself and the ones you love. This is particularly true of oral cancer, which is very treatable if caught early. Unfortunately, about two-thirds of oral cancers are not caught until the late stages. You may think that if you are a non-smoker, particularly a young one, this topic is not of concern to you. If so, please think again.
While most oral cancer patients are smokers, the fastest-growing segment of newly diagnosed cases is young, non-smoking adults. The culprit is a particular strain of the Human Papilloma Virus (HPV). HPV is the most common sexually transmitted disease in the U.S., with about 20 million Americans infected. In fact, it is estimated that at least half of all sexually active people will contract it during their lives. Most strains (and there are over 100) lead to symptoms no more serious than warts, and in many cases a person's own immune system can rid the body of the disease within two years. The strain known as HPV16, unfortunately, is different. By inserting its own DNA into human cells, the virus can cause a mutation that turns normal cells into malignant ones. You may already be aware that HPV16 has been linked to cervical cancer. We now know it is also responsible for many new cases of oral cancer.
Signs & Symptoms
Most of the lumps, bumps, and occasional sores you find in and around your mouth are completely harmless. But you should look out for changes such as white or red patches, ulcers and lumps anywhere in and around your face and neck that persist for more than a couple of weeks. A persistent sore throat or hoarseness is also cause for concern. Most oral cancers are “squamous” (scale-shaped) cell carcinomas. The sides of the tongue are the mostcommon sites for these small lesions. Because the tongue has a rich blood supply and a direct connection to the lymphatic system (a part of our immune system), it's a site from which cancer can easily spread. The floor of the mouth under the tongue is the second most common site. Cancerous lesions on the lower lip, which are usually preceded by chronic sun exposure, are not uncommon.
Diagnosis & Treatment
Regular screening for oral cancer is one of the most important services provided to you at the dental office. Your regular dental checkup includes a visual and tactile (touch) examination for any signs of oral cancer or precancerous lesions in and around your mouth and throat. Anything that looks suspicious, may be analyzed with a routine procedure called a biopsy, in which a small amount of the suspicious tissue is sent to a laboratory for microscopic inspection. This is the best way to get a definitive diagnosis. Should the lesion turn out to be cancerous, the rest of the malignant tissue will be removed. It's possible that radiation and/or chemotherapy will be needed to eradicate the disease. As mentioned before, when treatment occurs early, the survival rates are excellent.
Prevention
There are lifestyle choices you can make to reduce your risk considerably. Giving up tobacco in all forms, along with alcohol are big ones. Avoiding risky sexual behavior is also important. Protect yourself from overexposure to the sun, and eat a healthy diet. Research has consistently found that a high intake of fruits and vegetables is protective against oral and throat cancer; a good diet will also bolster your immune system. And please remember to schedule regular checkups here at the dental office.An oral cancer screening takes just a few minutes, but it could save your life.
Related Articles:
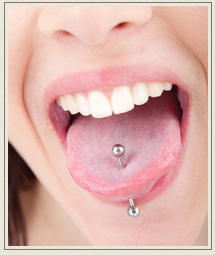
Oral Piercings
At the present time, oral piercings such as tongue bolts, cheek studs, and lip rings seem to be in vogue among a certain number of young people. Whether you find these bodily adornments appealing or repulsive is a matter of personal taste — but whichever side of the fashion divide you're on, there are a few things you should know about the impact they can have on your oral health.
According to the Journal of the American Dental Association, the tongue and lips are the most common sites for intraoral piercings. In either location, the ornament is likely to come into contact with teeth, gum tissue, and other anatomical structures in the mouth. And that's where the trouble may start.
The Anatomy of a Problem
The tongue, composed primarily of muscle tissue, is rich in blood supply and nerve endings; that's why a cut on the tongue is often painful and bloody. In a tongue piercing, a metal stud is inserted through a hole made in the tongue. The possibility of infection or the transmission of a blood-borne disease like hepatitis B exists in this situation. Rarely, the piercing may also cause immediate and severe facial pain. It's the long-term effects of an oral piercing, however, which give the most reason for concern.
As teeth regularly come into contact with the metal parts of the ornament, increased tooth sensitivity and pain may become a problem. Chipping or fracture of the teeth can also occur, which may require tooth restoration. Teeth that have already been restored (with crowns, for example) may be even more prone to damage. Plus, wherever it's located, jewelry in the mouth can trigger excessive saliva flow, impede speech, and cause problems with chewing and swallowing.
Periodontal (gum) disease can also result from wearing an oral piercing. This may first show up as injury to the soft gum tissue, and later as gum recession. It's important to understand that before the gums can recede, some of the underlying bone in the jaw must be lost. Following bone loss, inflammation and infection of the gums may occur.
When gums recede, tooth roots become exposed; this makes tooth decay more likely, since roots lack the protective enamel covering of the tooth's crown. Some studies have even shown that, over time, this condition makes gum disease more likely — primarily because it's more difficult to practice good oral hygiene with an irregular gum line. Besides causing problems in the mouth, advanced gum disease can have a potentially negative effect on your general (systemic) health.
It's Your Health — and Your Choice
If you're old enough to get an oral piercing, you're old enough to take an active part in maintaining your own oral health. If you are thinking about having a tongue bolt, lip ring, cheek stud, or other ornament placed in your mouth, talk to a dental professional about it first. Due to the increased potential for dental or periodontal problems, you will likely need to have more frequent checkups, and pay special attention to your oral hygiene.
And if the time comes when you decide that the piercing you got on an impulse isn't what you want any more, take heart: Removing it will immediately reduce your disease risk, and thus instantly improve your oral health!
Related Articles:
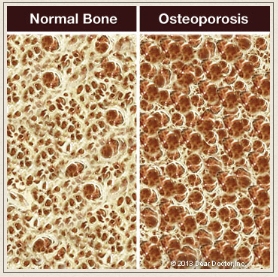
Osteoporosis & Oral Health
Osteoporosis is a condition that weakens bones and makes them more prone to fracture. Estimated to affect about 10 million Americans at present, it causes some 2 million fractures each year — and as our population ages, these numbers are expected to increase. Osteoporosis can affect any part of the body — including the jawbone that supports the teeth.
This may be of particular concern if you are considering certain dental procedures — for example, getting dental implants to replace missing teeth. Implants are today's gold standard for tooth replacement, because they look and function so much like real teeth. But their success depends on a process known as osseointegration, by which they fuse to living bone in the jaw. For this to occur, that bone must be relatively healthy; yet osteoporosis — and certain medications used to treat it — may affect your oral health.
Bone: An Ever-Changing Tissue
The living bone tissue in the body isn't like the dry, white skeleton you may have seen in a doctor's office or on TV. It is constantly being remodeled by two natural processes: resorption, in which the body removes and breaks down old, damaged bone; and bone formation, where the removed material is replaced by new, healthy bone. In an ideal situation, both processes happen at an equal rate; osteoporosis, however, tips the balance toward resorption, weakening the bone structure.
A class of drugs called bisphosphonates (whose brand names include Fosamax, Boniva, Reclast and Prolia) can inhibit resorption and help bring the two processes back into balance. But for reasons that aren't fully understood, these medications sometimes have a different effect on the bones of the jaw. In rare cases, long-term bisphosphonate users experience osteonecrosis of the jaw (ONJ), a condition in which isolated areas of jawbone lose their vitality and die. If you are acandidate for oral surgery, tooth extraction or implant placement, it's important to consider the possible effect of bisphosphonate use before you have this type of procedure.
Taking Medication
Over 90 percent of the people who suffer from bisphosphonate-associated ONJ received high doses of the medication intravenously — often for cancer treatment. Only a small percentage of those who take the drug orally are likely to develop this condition. So generally speaking, if you have osteoporosis or are at high risk of bone fractures, the benefit of taking these medications far outweighs the risk.
But if you are about to begin therapy with high doses of bisphosphonates, it's ideal to have a dental exam and resolve any oral disease before beginning the medication. Likewise, while you're receiving the medication, it's best to avoid invasive dental treatments if possible. However, since untreated oral disease may cause serious health problems, be sure to discuss the situation with all members of your medical team before making treatment decisions.
Most people who take oral bisphosphonates for osteoporosis won't have to postpone or avoid dental procedures, because they have little risk of developing ONJ. In the case of dental implant placement, the decision to proceed is made on an individual basis, after a thorough examination of the quality and quantity of tooth-supporting bone in the jaw. The presence of osteoporosis may influence the type of implants used, and the amount of healing time needed to complete the osseointegration process.
No matter what dental procedures you are considering, it is vital to keep us informed about any medical conditions you have, and any drugs you may be taking — both prescription and non-prescription.
Preventing Osteoporosis
There are several ways you can help prevent osteoporosis. For a start, make sure you're getting enough calcium and vitamin D. It also helps to decrease your caffeine and alcohol intake, and quit smoking. Weight-bearing exercise — physical activities that force you to work against gravity, like walking, jogging or weight training — can bring a host of benefits. And don't forget your regular visits to the dental office. Your dental professionals don't just help you to maintain good oral health — we encourage you to keep up your overall health as well.
Related Articles:
Pregnancy, Hormones & Oral Health
You probably know that many physical and emotional changes you will experience during pregnancy result from an increase in the levels of certain hormones — the chemicals that regulate many important processes in the body. But what you may not realize is that these hormonal variations can affect your oral health — and usually not for the better. In fact, surges in the female hormones estrogen and progesterone can dilate (expand) the tiny blood vessels in your gums, increasing blood flow. This makes gums more sensitive to the bacteria (and associated toxins) found in the sticky dental plaque that accumulates on teeth every day.
Pregnant women commonly notice that their gums may become red and swollen, and even bleed when they floss or brush their teeth, a condition known as “pregnancy gingivitis.” Similar gum inflammation can result from taking birth control pills that contain a type of synthetic progesterone, or even from the normal hormonal fluctuations of the menstrual cycle.
Another, less common effect of pregnancy hormones on the gums is an overgrowth of gum tissue or small, berry-colored lumps at the gum line or between teeth. These growths are called “pregnancy tumors,” though they are completely benign.
All of the above conditions usually clear up within a few months after giving birth. Still, if you experience gum inflammation, it's a sign that you need to take extra conscientious care of your teeth and gums during pregnancy.

Why It Matters
Pregnancy hormones don't cause gingivitis by themselves — the irritants in plaque need to be present first. So if you experience the signs and symptoms mentioned above, you'll want to redouble your oral hygiene efforts, both for your sake and your baby's. Untreated gingivitis can progress to a more serious form of gum disease called periodontitis — a bacterial infection that attacks not just the gums but also the tooth-supporting bone beneath. It can eventually cause bone loss, loose teeth and even tooth loss. Some research has even indicated a link between periodontal (gum) diseases and other serious health conditions, such as cardiovascular disease and diabetes.
Pregnant women should also be aware that studies have suggested a link between periodontal (gum) disease and preterm delivery. Although the exact mechanism by which this happens is unclear, evidence suggests that the bacteria in dental plaque can reach the placenta and trigger inflammatory responses. This causes substances to be released into the bloodstream that may in turn start labor prematurely. Preeclampsia, a form of high blood pressure specific to pregnancy, may also be associated with periodontal disease.
What You Can Do
* Eat right.
Even if pregnancy cravings are driving you to seek out sugar, try to go easy on the sweets. While they offer you and your developing baby virtually nothing in the way of nutrients, they're the favorite food of disease-causing oral bacteria. If you find you can't resist sweets, try to eat them only at mealtimes and make sure to brush your teeth afterwards.
* Stick to a good oral hygiene routine.
Make sure to floss every day and to brush your teeth at least twice per day. If morning (or afternoon or evening) sickness is a problem, don't brush immediately after throwing up. That's because the enamel on your teeth, which has been temporarily softened by the acid coming up from your stomach, can now be easily removed. Instead, rinse with a teaspoon of baking soda dissolved in a cup of water (or even plain water) to neutralize the acid. Wait a full hour before brushing your teeth.
* Have a dental cleaning and exam.
Not only are professional cleanings safe during pregnancy, they're highly recommended. So if you haven't been to the dentist in a while, now is a great time to make an appointment. And don't forget to share the happy news! You teeth can certainly be cleaned and examined — but for other non-emergency dental procedures, it's probably best to wait.
Related Articles:
Preventive Dentistry
You've no doubt heard it said that an ounce of prevention is worth a pound of cure. In dentistry, you might say it's worth two pounds. Maybe even thousands of dollars. That's because dental problems can become exponentially more expensive — and painful — the longer they go unaddressed. Fortunately, modern dentistry has many easy and relatively inexpensive ways to make sure that today's minor annoyance does not turn into tomorrow's major headache.
Preventive dentistry describes all the procedures used to arrest tooth decay and other diseases in the earliest stages. The goal is to keep you as healthy as possible and maintain your natural teeth for life.
Preventive Dentistry Procedures
Preventive dentistry procedures range from the most basic services that have been used successfully for decades, to recent technological innovations. These procedures include:
* Cleanings.
This is where dental health starts. There's just no substitute for physically removing disease-causing dental plaque and calculus (tartar) from your teeth — especially in hard-to-reach areas near the gum line. That's why regular professional cleanings are so important to your health.
*Dental Sealants.
These invisible plastic coatings fill the tiny grooves in back teeth so they do not become havens for bacteria. They prevent cavities from forming and the need for fillings later on.
* Fluoride.
This mineral is readily incorporated into the teeth's mineral structure, thereby making them stronger and more decay-resistant. Fluoride can even reverse tiny cavities that are starting to form. If you are not getting enough from your toothpaste and drinking water, it can be applied directly to your teeth at the dental office.
* Laser Decay Diagnosis.
Laser light can be used to detect early tooth decay quickly and easily, right in the dental office — before full-blown cavities form.
* Mouthguards.
Athletic mouthguards are designed to absorb and distribute the forces of impact and minimize traumatic injury to both the hard and soft tissues of the mouth. In fact, an athlete is 60 times more likely to suffer harm to teeth when not wearing a mouthguard. The best ones are custom-made for you by your dentist.
*Oral Cancer Screenings.
Your best chance of surviving oral cancer — a disease that affects not only lifelong smokers but also young non-smokers — is early detection and treatment. Oral cancer screenings are a routine part of every regular dental exam.
* Salivary Diagnostics.
This is an exciting new development in the field of preventive dentistry. While it is in its infancy, it is already possible to detect the presence of certain diseases with a salvia test, and the technology is developing rapidly.
* X-Rays.
For around a century, dentists have been using x-rays to reveal signs of disease not visible to the naked eye. Now, with CAT scans, they have become three-dimensional and are an indispensable tool to diagnose tooth decay, gum disease, bone density, bone volume and tumors.
Your Role in Preventing Dental Disease
There's one more extremely important component of preventive dentistry: you. The procedures mentioned above can only be effective if you come in to the dental office to take advantage of them. Likewise, the importance of maintaining a good oral hygiene routine at home cannot be overstated. Daily effective brushing and flossing will go a long way toward removing the dental plaque responsible for dental disease, tooth loss, and the need for more complex dental treatment.
Related Articles:
Professional Teeth Cleanings
Even if you brush and floss your teeth faithfully, it is important that you have your teeth professionally cleaned on a regular basis. (Of course, if you aren't quite so meticulous about your oral hygiene, it's even more important!) After a thorough cleaning, your teeth will feel smooth and squeaky-clean, and they will probably look a lot brighter too. But professional teeth cleanings aren't done for looks alone. Why do your teeth need this kind of attention? Essentially, it's because over time they tend to build up a layer of plaque (a sticky, bacteria-rich film) and hard deposits (called tartar, or calculus) that are very difficult to remove without special tools. When these deposits are allowed to remain on the tooth surfaces or below the gum line, they provide ideal conditions for bacteria to grow and multiply. The acids produced by some bacteria cause tooth decay and gum disease; if left uncontrolled, this can lead to inflammation and infection of the gums, and possibly influence systemic (whole body) diseases.
Dentists have a special term for preventive procedures like tooth cleaning: prophylaxis, from the Greek word meaning to protect or guard against. In this case, the focus is on preventing tooth decay and gum disease. Performed in conjunction with a routine dental examination, a professional cleaning can go a long way toward controlling these two common maladies. While your teeth are being cleaned, it's also a good opportunity to take a close look at your oral health in general and check for a few specific problems.
The Professional Cleaning Procedure
Teeth cleaning is often performed by a dental hygienist — a highly trained technician who uses a special set of tools designed just for this purpose. Because everyone's teeth are a little different, your cleaning will be tailored to your particular needs. However, many cleanings follow a similar pattern.
First, the dental hygienist will do an oral examination to evaluate the health of your oral tissues. Then the cleaning will take place using either an ultrasonic scaler or metal instruments referred to as curettes to remove the plaque and calculus from the tooth surfaces. The ultrasonic scaler is a hand-held tool with a tiny tip that vibrates at a very high frequency. Hardened deposits are broken up by the rapid movement of the tip, which does not damage the tooth. A constant stream of liquid (called lavage) serves to cool the tip and aid in plaque removal; at the same time, it also washes away the debris.
Some hygienists prefer curettes, which are hand-held instruments that are curved and tapered to fit around and in between the teeth. If your teeth are sensitive, using hand-held instruments may be more comfortable for a professional cleaning. In the capable hands of a hygienist or dentist, it takes only moderate pressure to remove any stubborn buildup and scrub the teeth clean, regardless of which instruments are used.
Finally, your teeth are polished with a low-speed rotary brush fitted with a soft rubber tip. A slightly gritty, toothpaste-like gel is applied, and the tip spins around and polishes the teeth, making them smooth and shiny.
A Requirement for Good Oral Health
Most people don't feel any noticeable discomfort during dental cleanings; some even report they enjoy the experience — especially the dramatic results when it's done! If you haven't had a cleaning in a while, however, it may take you a few moments to get used to getting your teeth cleaned. If you experience any discomfort, however, it may be possible to apply a topical numbing gel or another type of anesthetic.
If your gums are irritated due to bacterial buildup, they may become sore or bleed slightly during the cleaning. It may be possible to prevent this from occuring in the future with oral hygiene measures you can perform at home (such as improved flossing techniques or special mouthrinses); it might also indicate that you need more frequent in-office cleanings. This type of regular maintenance will help you avoid more involved dental procedures down the road — and it will give you the best chance of keeping your teeth for life!

Related Articles:
Stress & Oral Habits
Teeth grinding and clenching are common habits, but that doesn't mean they are harmless. Stresses from the powerful forces generated by grinding and clenching (also known as “bruxing”) can wear down teeth or even loosen them. Teeth that have enamel worn away or scraped off from this repeated rubbing action may become sensitive to hot or cold. And dental work such as crowns and fillings may get damaged. Bruxism can also lead to jaw pain and/or headaches.
Even if you have experienced some of these signs and symptoms, you may not realize you are a bruxer — particularly if your habit is nocturnal, as is often the case. Yet the evidence of tooth damage may become obvious during your regular checkup and cleaning. Dentists can also help you break the habit, relieve any pain you are experiencing, and repair any damage to your teeth or dental work.
Why do we grind or clench our teeth?
The most common reason for grinding/clenching habits is stress, which can affect our health in various ways. Some people experience stomach pain or skin breakouts; bruxing is yet another manifestation. Sometimes people grind their teeth because of misaligned teeth or other bite problems. Using stimulating substances such as caffeine, alcohol, tobacco and illegal drugs can also put you at risk. Additionally, teeth grinding is believed to be an uncommon side effect of certain medications.
What can be done?
Sometimes simply becoming aware of the habit can help you to get it under control. If stress is the issue, try to find healthy ways of managing it: exercise, meditation, listening to relaxing music, or a warm bath may help. Your teeth will be monitored over time at the dental office to make sure the problem is not worsening.
If damage to your teeth or existing dental work is evident, we may recommend a custom-made nightguard, also known as an “occlusal guard,” may be recommended. It resembles an athletic mouthguard. Made of comfortable plastic, the guard is worn at night to keep your teeth from actually contacting each other. It also helps protect your jaw joints from excessive force.If a bite problem exists where some teeth are hitting before the others (all of your teeth should hit at the same time), it can sometimes be treated by removing a tiny bit of enamel from an individual tooth that is sticking up a bit (and therefore receiving too much force) to bring it in line with the others. This is known as a bite adjustment. If your malocclusion (bad bite) is more serious, orthodontics might be recommended. Replacing any teeth that are missing can also help stabilize your bite by inhibiting the shifting of teeth that occurs when extra space is left open by missing teeth.
A word about kids:
Teeth grinding is very common in children, especially when they are shedding their baby teeth. Since they often outgrow it, treatment is not usually recommended.
Related Articles:
Our Facebook Feed
Privacy Policy
| Do Not Share My Information
| Conditions of Use
| Notice and Take Down Policy
| Website Accessibility Policy
© 2024
The content on this website is owned by us and our licensors. Do not copy any content (including images) without our consent.

